People with severe mental illness are waiting for days in hospital EDs. Here’s how we can do better
- Written by The Conversation
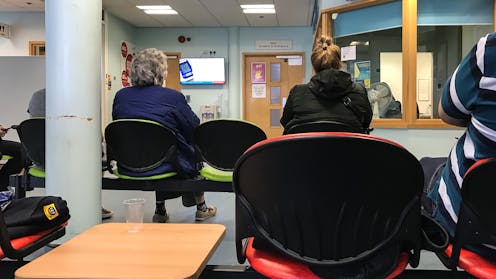
On ABC’s 4 Corners this week, psychiatrists and nurses have warned New South Wales’ mental health system is in crisis. They report some patients with severe mental distress are waiting two to three days in emergency departments for care.
The program highlighted chronic failures in NSW’s mental health system, but the shortfalls are being felt across the nation.
Just over 7% of the nation’s health budget is spent on mental health. But together with alcohol and drug issues, mental health accounts for around 15% of the nation’s burden of disease.
Problems in mental health go beyond under-funding: it’s also about how the resources we do have are spent.
So how did we get here? And what can we do to fix it?
It wasn’t supposed to be like this
Back in the 1980s, psychiatric deinstitutionalisation promised to replace treatment provided in the old psychiatric institutions with mental health services and care in the community. Too often, these institutions failed to promote recovery, and delivered improper care and even abuse.
Many of these institutions were indeed closed. But the shift in mental health care over the past 40 years has not been from asylums to the community, but rather to the mental health wards of Australia’s general public hospitals and the emergency departments (EDs) which operate in them.
Hospitals are expensive and often traumatic places to provide mental health care. We know this from frequent statutory inquiries and reports.
For presentations to EDs, all the indicators are heading in the wrong direction. More people are seeking care for their mental health in EDs, they are arriving sicker (according to their triage category) and they wait longer for care.
Hospitals account for more than 80% of total state and territory spending on mental health. In 2022–23, A$6.5 billion of the states and territories’ total spend of $8bn on mental health was directed towards hospital-based care. Just $1bn was provided outside hospitals.
Evidence indicates community-based care can reduce reliance on EDs for mental health care.
Yet community mental health services now often comprise little more than a phone call to check if a client is taking their medication. Of the 9.4 million community mental health service contacts in 2022–3, 4 million lasted less than 15 minutes.
Mental health clinical staff spend just 20% of their time with consumers.
What are the solutions?
The solutions are already at hand, but haven’t been pursued or scaled up. These include:
multidisciplinary models such as assertive community treatments, which provide mixed specialist clinical and psychosocial support in the community, in people’s homes
service models the Australian College of Emergency Medicine have proposed as alternatives to hospital ED care. These include safe havens, mental health nurse liaison services and dedicated homelessness teams. These services can provide the care required to divert patients away from hectic emergency departments, in calmer, more therapeutic spaces
NSW programs such as the Housing and Accommodation Support Initiative provide community based, clinical and psychosocial support to people with severe mental health needs. This program reduced admissions due to mental health by 74% over two years
Adelaide’s Urgent Mental Health Care Centre, which operates as an alternative to EDs and is open 24 hours a day, seven days a week. This clinic was designed in collaboration with the community, including people with a lived experience of a mental health crisis, and offers a welcoming, safe environment
Step-Up Step-Down services, which can effectively meet the needs of some of “the missing middle”. These are people whose mental health needs are too complex for primary care but not assessed as a big enough risk to themselves or others to “qualify” for hospital admission.
Funding support for psychosocial services remains tiny. It accounts for about 6% of total spending on mental health care by states and territories.
As a result, almost half a million Australians with either severe or moderate mental health needs are currently unable to access necessary psychosocial care. This impacts their recovery.
It also leaves clinical services without a viable “psychosocial partner”. So people needing mental health care might be able to get a prescription, but are much less likely to receive assistance with unstable housing, employment support or help getting back to school.
Working together
There is already concern to address identified workforce shortages and psychiatrists’ pay disputes.
The next round of mental health planning must also discuss and clarify the complementary roles in mental health care, as people with more complex mental health needs typically benefit from multidisciplinary, team-based care. This includes psychiatrists, psychologists, allied health professionals, nurses, peer workers, social service providers, GPs, justice, school and housing services and others such as drug and alcohol services. Who is best placed to plan and coordinate this care?
Reducing our over-reliance on hospital-based mental health care and EDs needs agreement by all Australian governments to explicitly prioritise the principles of early intervention, community-based mental health care and hospital avoidance in mental health.
These steps, together with more personalised approaches to treatment and better accountability, will help us achieve systemic quality improvement in mental health care.







